



features
Magellan member satisfaction survey results highlight providers' impact
Magellan cares about the members we serve, and we know you do, too. In the ongoing effort to improve the quality of our programs and services, we conduct an annual survey that gives members across the country an opportunity to weigh in on areas of service that they are happy about and where they notice the need for improvement.
We measure rates of satisfaction across multiple domains such as accessibility of care, timeliness of service, convenience of appointment times, responsiveness of the therapist, helpfulness of our customer services, and other areas comprising the treatment experience.
Analysis of feedback by plan type highlights the strengths and opportunities for each:
Commercial and employer health plans (not in California)
- Strengths: Providers offering services at times that are convenient for members; Access to quality healthcare
- Opportunities: Improve member’s choice of providers and services covered
Employee Assistance Programs (EAPs not in California)
- Strengths: Service quality (in-person counseling); dealing with concerns effectively; counselor’s ability to listen and understand concerns
- Opportunities: Improve member’s choice of counselors
California commercial health plans
- Strengths: Access to quality healthcare; member’s improved mental health
- Opportunities: Increase covered services and choice of providers
California Employee Assistance Programs (EAPs)
- Strengths: Service quality (in-person counseling); counselor’s ability to listen and understand concerns
- Opportunities: Improve member’s choice of counselors and ability to deal with concerns more effectively
3 components of member experience that shape overall satisfaction
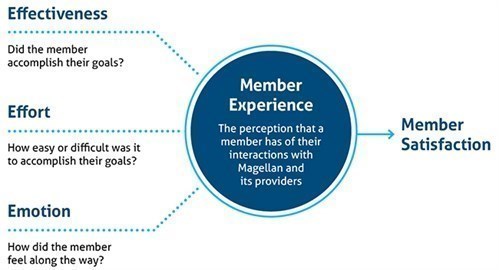
Meeting members’ needs is the most important component of a positive member experience, but meeting needs isn’t enough to guarantee high member satisfaction. The process should be easy and pleasant, too.
Members consider a variety of factors when evaluating their satisfaction with services provided by Magellan. The quality of care is extremely important, but they also think about the effort they expended to access that care, and all the emotions they experienced throughout the process. Members generally rate the quality of care received by providers and counselors highly. But there are opportunities to make it easier to access that care.
What providers can do to improve members' satisfaction with access and getting needs met
- Review policies/procedures to identify any unintentional consequences that cause delays in accepting new patients.
- Identify barriers in office settings and community related to access and use quality improvement processes (such as Plan-Do-Study-Act) to test changes related to community collaboration, communication, screenings, appointment setting, follow up and care planning.
- Book the member an appointment at first call to your office.
- Create a hybrid approach to treatment with face to face and telehealth options available.
- Ensure the utilization of language services.
- Collaborate with primary care providers to screen and identify needs prior to crisis.
- Work with local and state boards of mental health and medical health care systems to participate in a central database for real-time access awareness.
- Keep practice information—including specialties, contact and availability—up to date via Magellan provider portal.
What providers can do to improve members' level of happiness with healthcare provider choices and convenience of care
- Encourage member health literacy through:
- clear communication
- check their understanding through teach back
- shared decision making
- easy to use platforms for members to access electronic health information
- evidence-based resources for members to seek self-management support
- Apply motivational interviewing strategies when working with members.
- Encourage support system involvement.
- Address concerns at time of visit or call with clear plans to follow up as needed.
- Review policies/procedures to identify any areas that may be unintentionally causing delay to receiving information, referrals, office wait time and utilization of screening tools.
Thank you for your commitment to meeting the needs of Magellan members and improving their satisfaction with the mental health, substance use, and EAP services they receive. We will continue to collaborate with providers to improve members’ experience and treatment outcomes.

